
Action Needed: Physician's Self-Prescription for the Wellbeing of Medicine
We are in a three-week series called Action Needed for the Wellbeing of Medicine. Last week we covered well-being from an organizational standpoint because we know that 80% of the contributors toward burnout are related to the systems. Today we are shifting our focus to the 20% that we have some control over to prevent and treat burnout and improve our own wellbeing.
First, let me start by saying I know you are already resilient. The rigorous process of premed, MCAT, medical school, and residency selects for resilience. Further, there are studies supporting physicians’ resilience.That doesn’t mean, however, that there aren’t steps you can take to improve your enjoyment of your career.
So, what can you do for yourself? Well, no matter if you’re thriving, surviving, or burning out, the first step toward an impactful and sustainable career is for each physician to care for and protect themselves.
I’m going to merge the various recommendations from the US Surgeon General’s 2022 advisory and the ACGME’s Well-being Guidebook and enhance them with wise words from Dr. Lex Von Hafften’s recent presentation mentioned last week, as well as my suggestions based on my personal, faculty, and coaching experiences. Think through each section as you read. In the end, I'll offer a couple of first steps so you don't heap more check boxes on your to-do list.
Time
Before you can do any of the following, you MUST carve out protected, prioritized time for yourself and honor it to do any of the following steps. In the hustle to check all the boxes, we physicians cut out “unnecessary, nonurgent, or softer” activities such as reflection. We have too much on our to-do list, and time is scarce.
If you think of it, it’s like pulling onto the road without pausing to look up an address or enter it into the GPS. Time is needed to think, reflect, process and plan.
How much time and how often do you want to begin? Put it on your schedule. What can you put in place to protect it?
Awareness.
Before developing a plan, we must uncover a few things.
- What are your tell-tale signs of increasing stress?
What feelings, emotions, or behaviors can serve as early clues of a worsening mental, emotional, or physical state before it hits crisis levels?
How do you know when you’re emotionally exhausted vs. physically?
How do you know when you are starting to disengage?
What types of things do you say to yourself when you are losing your belief in your personal efficacy?
Who knows you so well that they often are the first to know something is off?
Make note of these key realizations so you can be on the lookout for them.
- Self-assessment.
- Checking in with yourself regularly can be incredibly helpful. This can be an easy Likert scale for your stress level, 1-10, and assessing at specific periods in your workday.
- Use longer-term metrics via validated tools periodically, such as the
- The Stress Continuum Model (adapted from the Navy to assess teams/individuals in combat).
- The Wellbeing Index Self-assessment
- The Oldenburg Burnout Inventory
- The PHQ9 Screen for Depression
- What are your most useful advantageous internal and external coping skills?
- What are your more harmful coping mechanisms? Take note of these as well. Begin to think of ways to shift toward the more adaptive ones more often.
I find that many I coach like the 2-pronged approach.
-Activating the parasympathetic with breathing exercises such as box breathing or 4-7-8 breathing
- Coming back to the present moment in time since much of our stress is based on anticipated negative outcomes or past ruminations. Activating your senses is a great way to come back to the present. What do you see, hear, feel, smell, or taste – use detailed focus on one at a time.
Connection:
We tend to turn inward when stressed and detach when burning out. Even before that point, some of us cut out socializing at work to check all the boxes. This was me. I worked in my office throughout lunch. I stopped asking people about their vacations, etc., in an effort to get more done. Paradoxically, it heightens the risk of burnout and harms our mental fitness. Trust me on this.
- With whom do you want to intentionally maintain or foster connection – at and outside of work?
- What are the various scenarios that allow for that to happen?
- What’s the right balance between socializing and working for you?
- Who are your trustworthy colleagues, friends, clergy, or mentors you could call if things get tough? Identify them now.
- What are the professional resources to which you have access?
- Structured peer support – with colleagues, mentors, and physician coaches
- Structured programs such as Balint groups, Finding Meaning in Medicine, and Schwartz Rounds
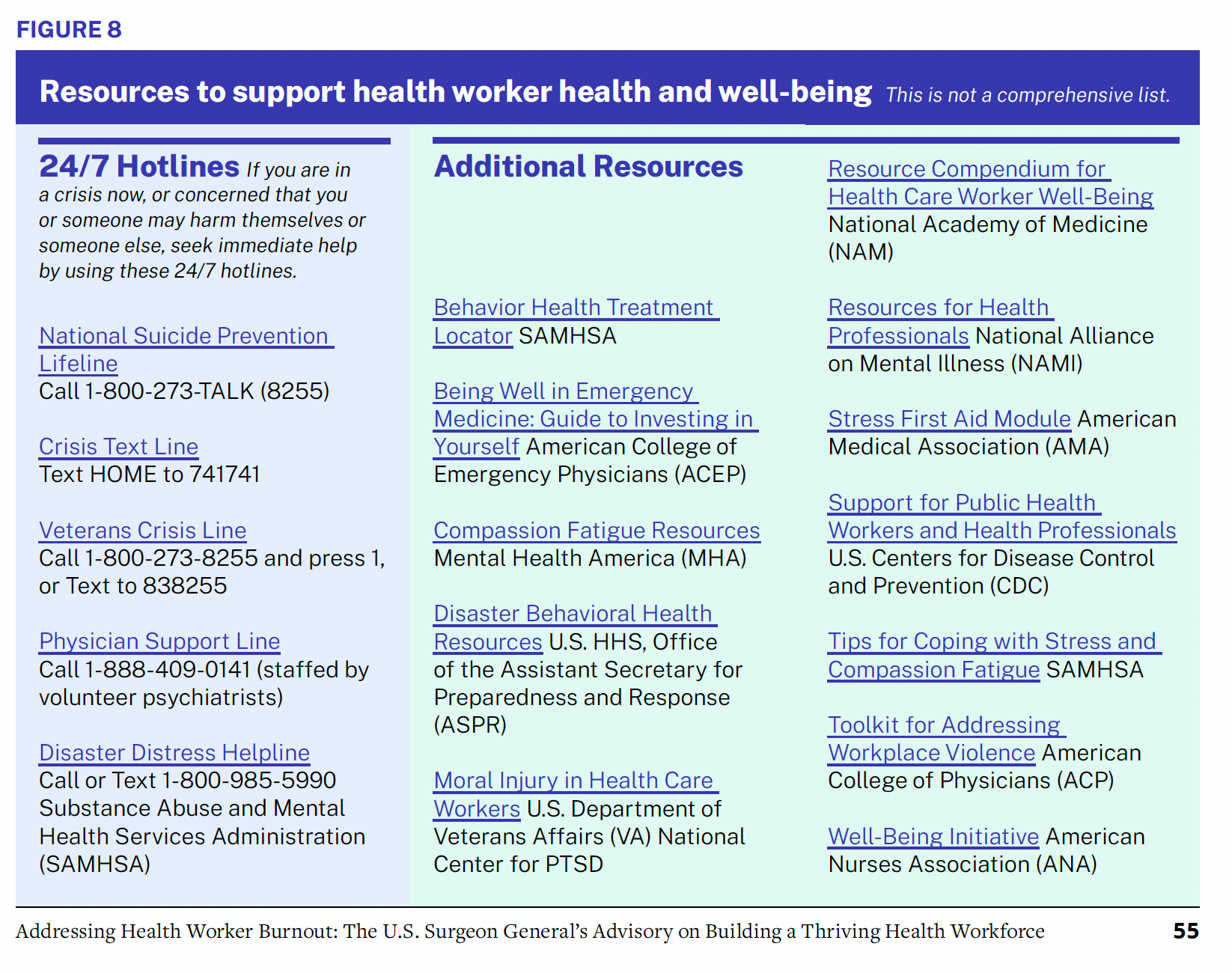
- Behavioral Health specialists – EAP options, your primary care physician, therapist, psychologist, or psychiatrist (resource table below).
Self-Care:
- Basic physical – what needs the most attention – sleep, movement, nutrition? What do you need to give yourself? What permission do you need to grant yourself to prioritize those?
- Psychological
- Basics – autonomy, competency, and connection (above).
- Where can you take back your agency? When stressed, we often give away our own power in things we can do. We reinforce the feelings of helplessness and turn to blame. However, there are often situations we could have more agency than we think when we get back in a clear mindset.
- What skills do you want to enhance in your work environment? Are there ways to gain efficiency? Do you want to play a role in changing the culture? What skills do you want to learn to do so? Are there skills you want to grow in related to mindset, coping, and soothing you want to learn? The ACGME podcast has a range of topics that include coping and self-soothing strategies to manage emotions and recover from emotional storms.
- Other proven strategies include Mindfulness-Based Stress Reduction (MBSR), CBT, and professional coaching.
- Using the data from your stress self-assessment, develop a protocol. It could look like this: If you hit a 5 or 6 on the Likert scale, you implement your calming and coping strategies. When you hit a 7 or 8, you reach out to that list of trustworthy people, take a time-out, etc. If it’s above an 8, make appointments with your professional resources. Or know your emergency plan if there isn’t time for an appointment. Using data from one of the validated tools, determine what activities you need to change up when you hit certain marks. You get to decide what works for you.
- Increase the activities that add meaning to your work. What aligns with your core values, purpose, and vision that fulfills you? What are the reasons you chose your profession? How can you get back to that? These are ways you can build back your self-belief and self-efficacy. We know if you can increase those activities or roles in your career, even if added in small increments up to 20% of your job, it benefits your wellbeing. What things at work still make you smile on the inside? Add to it each month. Don’t let your brain off the hook when it offers, “there’s nothing I can do.” Put it on task to think outside the box and advocate for small meaningful changes for yourself. It’s a process, but moving the needle even 1% in the right direction will add up over time.
- What are other activities you want to put time and intention toward bringing joy to your life? Look for ways to combine them, such as physical activity outdoors in nature with friends or family.
- Remember – Good self-care not only helps you but others as well. When you are healthy, as opposed to burned out, you are more present, effective, and efficient personally and professionally. It changes how you interact with loved ones. It helps your team. It reduces the risk of errors, malpractice risks, and admissions. This enhances your efficiency, quality of patient care, patient safety, and satisfaction. So, in no way is it selfish to prioritize the things you need.
- Basics – autonomy, competency, and connection (above).
Advocacy
What areas do you want to advocate for yourself (and your colleagues, your team, and your patients?)
- Workload, work compression - more time for patients, more admin time, more same-day acute-care appointments, etc.
- Resources for efficiency - Hands-on EMR efficiency tips, a scribe, an efficient computer, upgraded Dragon, quiet space to dictate between patients, etc.
- Feedback about culture - Townhalls, open access to directors and CEO's, luncheons with those empowered to make change, anonymous venues to report, etc.
- Social support - Changes in the department's schedule or space to enhance natural socialization, organized events, structured peer-to-peer individual, group, or coaching support, etc.
- Mental health support - effective EAP, time for appointments, mental health days included for PTO, an encouraging culture around mental health instead of a shaming one, etc
- Others?
How do you get started?
Okay, so first steps - with all the above reflections,
1. Make a little notecard as a “Distress Go-Kit,” designed by the ACGME:
My wellbeing plan:
- My warning signs-
- My healthy soothing and internal coping strategies-
- People or social interactions that may provide a good distraction-
- Those I will call for help -
- Who are the professionals/agencies I will seek help from –
Write your protocol from the self-care part 2 section above on the back.
2. Decide what is one next small step in one arena above you want to make today.
Next week we will discuss what you can do for a colleague, friend, or family.
Look for the joy this week! Tonya
Download the first three key steps I recommend to increase your joy now in your life and career. Click here
If this topic resonated with you, you’d probably enjoy Weekend Reads — a short, thoughtful email I send each week with ideas and tools for physicians learning to cope, lead, and thrive.
Join Weekend Reads
Join Weekend Reads
Weekly insights, tips, and tools for physicians who want to thrive—plus a dash of fun.
We hate SPAM. We will never sell your information, for any reason.

