
Faculty Coaching Skills - Part 3 Partnering to Define and Design Progress
This post is part of the Faculty Coaching Skills Series, which explores how faculty can apply coaching approaches in medical education.A couple of weeks ago, we walked through an overview of and covered the first, Creating a Safe Space, followed by last week’s Deep Listening and Developing Awareness. This week, we will take a deeper dive on the skill Partnering to Define and Design Progress.
I want to offer that not every situation calls for a coaching approach. It will often still serve you and the trainee best to take the expert advice-giving faculty member in many situations. Trust the experiment of learning when to use and practice your coaching skills, in which situations, and with which learners.
The ability to flex between approaches—directive, performance-focused, or developmental—sits at the heart of the Adaptive Coaching Spectrum. Some moments call for clear guidance; others for space to think aloud. The artistry is in reading the learner and context, then adjusting your stance. Most of what follows fits within the Co-Creation Zone—where you and the resident share ownership for defining what progress looks like.
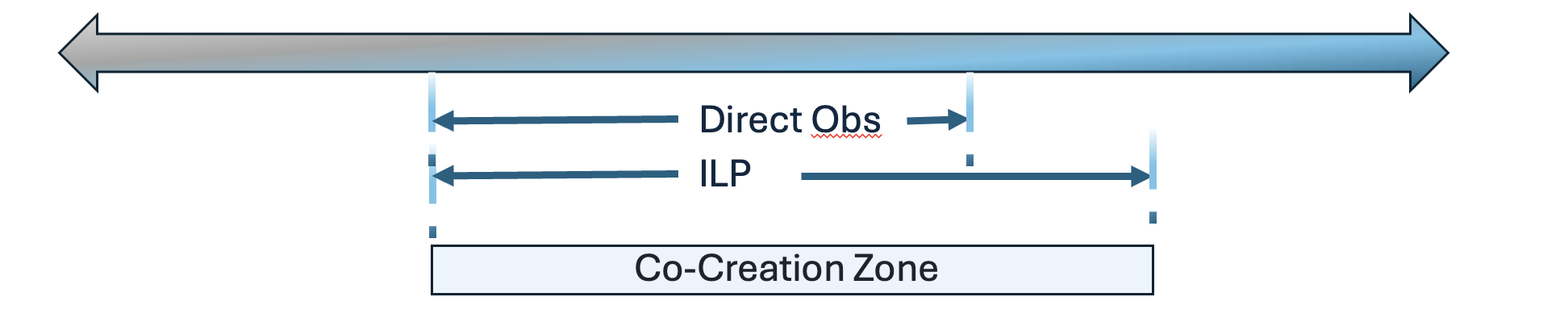
As mentioned previously, I want to push you more toward creating space for your residents to explore their perceptions and ideas. This will help them gain both the skills and the confidence to utilize metacognitive skills and stop over-relying on others for advice, especially in the more developmental areas such as the ILP. I will continue highlighting aspects that may feel new, challenging, or uncomfortable.
Skill Outline Review:
- Create a Safe Space
- Deep Listening
- Develop Awareness
- Partner to Define/Design Progress
- Assist Internalization of Learning
- Assist Accountability Plan
Partnering to Define and Design Progress.
Partnering as a faculty member, as opposed to a professional physician coach, is a joint effort – it’s co-created, though it remains trainee-centric. In today’s blog, I’m focusing on residents who don’t require program intervention and probation. For more information on remediation, look at the ACGME Remediation Toolkit which even offers several coaching frameworks.
Defining Progress:
It is important to allow the learner to think through what progress means to them in the context of the situation. Whether it’s figuring out how to respond to formative feedback, managing their time in clinic, or growing in their clinical decision–making, allowing space for them to self-assess, reflect, and define progress is crucial in the educational alliance of developing Master Adaptive Learners.
Listening for how they describe progress can help you gauge where they are on the spectrum—do they need more direction, affirmation, or space to think aloud? And remember, psychological safety underpins this process; residents engage more honestly when curiosity isn’t mistaken for incompetence.If they are progressing as expected, or even if there are early or initial concerns, the prerogative still lies with the learner for routine or corrective actions.
Once they’ve defined progress, you can offer your edits or suggestions to consider. After all, you have the expertise and better perspective on what’s needed. But allowing them to explore first is very useful—for their motivation and for your understanding of where they are. That back-and-forth is exactly what keeps the conversation in the Co-Creation Zone—balancing faculty guidance with learner ownership.
When a resident is in danger of needing remediation, you will want to be explicit about defining progress and transparent about the level of concern while still supporting choice within defined options.
Designing Progress:
Michael Bungay Stanier wrote a management book called The Advice Trap in which he talks about all of us having advice monsters.
Your own personal advice monster will likely show up loud and proud during this stage of the conversation. I invite you to quiet your monster and put it on the back burner while empowering your resident to formulate ideas.
Partner with residents to create SMART goals, even outside an ILP, when appropriate. For example, in clinic maybe they identify they want to be more on time. What specifically do they want to do to address that, how can they measure it, how can they make that goal more achievable, etc.
You can ask what they see as the most significant contributor to running behind and what ideas they address it. Like most of us, you will often find that our trainees are overachievers and sometimes set lofty goals (“My goal is to walk into all patients’ rooms within 5 minutes of their appointment time”). It’s a great goal and may even be achievable at some point, but if they’re consistently running 45 to 90 minutes behind, it’s not yet the short-term goal to work toward. You can normalize dialing down the idealism to help it be more achievable (“What if you consider initially making the goal 10% better than where you are now, what would that look like?”)
Explore Motivation:
What is their level of importance, confidence, and readiness on a scale of 1-10? What would they need to get each of those up to 7? (or 1-2 points better if they’re far off).
Plan for Obstacles:
What obstacles do they anticipate in meeting their goal? Demonstrate that every obstacle is a strategy waiting for discovery. What ideas do they have to overcome those? How will they utilize their strengths and resources to overcome them? What additional resources will they need?
Permission to Experiment:
What’s the first step or next step they need to try? Small steps take less activation energy. Use language to show them they’re in a PDSA cycle. They will learn from each attempt and then tweak or rethink. By receiving permission to try things, they will have less fear of failing to meet the goal, lowering the risk of procrastination.
Negotiating and Advice:
There will be clear times when you must permit your monster to speak and offer advice.
- Negotiation is needed. When they fail to consider important facts, limitations, or feedback, you would be doing them a disservice not to speak up. And it would be torture to try to ask them leading questions to the answer you’re looking for. So, it’s an appropriate time to offer guidance. (“I know your clinical knowledge was identified as an area of needed growth by some recent feedback. And I’d like to point out that your goal of clinic efficiency will be helpful in supporting that goal in tandem. I’d like to suggest that you look up one short clinical question for half of your patients during the session at the point of care. What do you think about that? How do we incorporate it? What would be more realistic or helpful?”)
- They genuinely don’t know. If you give them space to think after they say they don’t know and you’ve asked them to guess, in service of the trainee – make your recommendations. (“I find reminding the patient I want to optimize our 20 minutes together kind and useful in helping them decide the most important topics for our visit. What are your thoughts about that? How can you tailor it to your style?”)
- They really want to hear your opinion and advice. I still encourage you to say something like, “I’ll be happy to give you my advice, but first, I’d love to hear your ideas.” But then, give your advice.
Remember, that taking a coaching approach and determining when it’s the best approach is a skill you are expanding. Lean in with courage and have fun as your residents surprise you with what they can uncover.
That’s all for this week. Next week, we finish up with the remaining coaching skill.
Until then, have a joy-filled week! Tonya
Residency programs can benefit from our Flagship 6-session hybrid coaching course for resident or faculty groups. Learn more here https://www.joyinfamilymedicine.com/residency-programs
Join Weekend Reads
Weekly insights, tips, and tools for physicians who want to thrive—plus a dash of fun.
We hate SPAM. We will never sell your information, for any reason.

