
Faculty Coaching: True Performance Coaching
We’ve talked a lot about developmental coaching in this Faculty Coaching Series - those deeper, reflective conversations that help residents connect learning to purpose, values, and wellbeing. But today, let’s look at performance coaching (aka skills-based coaching), the kind that happens right in the clinical trenches: teaching moments, direct observation, and formative feedback.
Performance coaching doesn’t mean being less “coach-like.” It’s about recognizing when the learner needs more structure, direction, and concrete feedback to improve a skill or behavior. The faculty coach’s role is to guide performance while developing reflection and self-direction, staying in what I call the Co-Creation Zone.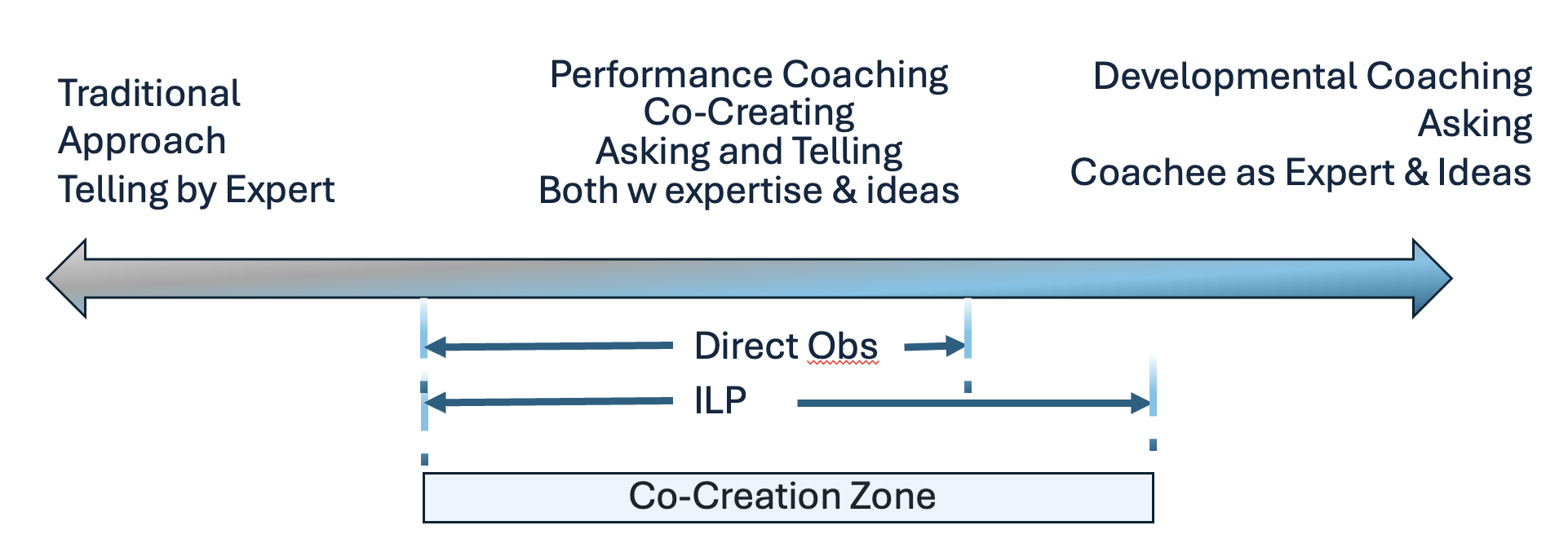
In this middle space of the Adaptive Coaching Spectrum, faculty and learners share expertise and reflection. The faculty brings clinical wisdom and feedback; the learner brings self-assessment, curiosity, and intent to grow. Coaching here helps residents take greater ownership of and deepen their learning without losing access to your experience.
Performance Coaching = Skills Building
Performance coaching is fundamentally about building skills.
Those skills span three interrelated domains:
-
Technical skills – procedural or psychomotor: suturing, airway management, ultrasound-guided procedures, or physical exam maneuvers.
-
Communication skills – explaining treatment plans, agenda setting, shared decision-making, or responding to emotion.
-
Cognitive skills – reasoning processes: formulating differential diagnoses, prioritizing next steps, or applying illness scripts efficiently in real time.
Many activities blend these categories.
For example, note writing and EHR use typically sit at the intersection of cognitive and communication skills, combining reasoning (organizing, prioritizing, synthesizing) with written communication for continuity and clarity.
If you’re coaching on workflow or documentation shortcuts, that leans more technical; if you’re coaching on how clearly the note communicates thinking, that’s cognitive and communication.
The Sweet Spot of Performance Coaching
When performance coaching really works, it lives in that shared space of inquiry and expertise.
Both you and the resident are engaged in a dialog, asking and telling, offering your expertise, bringing out their insights, trading perspectives, and building understanding together. You’re contributing your experience while drawing out theirs, creating what David Schön called the reflective conversation on the situation. This is turn will help them get better at reflecting in the moment, responding in real time.
In this moment, both teacher and learner are become atuned to the “surprise”, those flickers of congitvie discomfort that mark the edge of growth. Schön described it as the surprise of knowing you don’t know. Coaching helps residents notice that moment of uncertainty, stay curious about it, and use it as fuel for reflection and adaptation.
This is the educational alliance at its most productive. Each person contributing insight, trust, and curiosity in real time. When you co-create the plan forward, you’re not just closing a feedback loop; you’re walking together through the Master Adaptive Learning (MAL) process that underlies sustainable growth in medicine.
The MAL Process in Practice
-
Plan: Identify a clear goal or gap to address, rooted in feedback or observation.
-
Learn: Engage in deliberate practice, through reading, simulation, or repetition, using spaced practice to strengthen retention.
-
Assess: Integrate self-assessment with external input. True informed self-assessment blends the learner’s reflection with data and others’ perspectives for a higher level of accuracy.
-
Adjust: Interpret what worked, what didn’t, and how to transfer learning to new contexts.
Each step builds the habits and skills (that aren’t natural for many of us) of self-reflection, self-assessment, and self-direction that physicians need to thrive amid the rapid evolution of medicine and technology. Coaching gives structure and support to that process so learners develop their own internal compass for improvement.
Turning Feedback Into Coaching Conversations
Frameworks give structure to these brief but powerful teaching moments. You don’t have to become a certified coach to have these conversation.
R2C2, Ask–Tell–Ask, and Prepare to ADAPT each offer a reliable rhythm for coaching within clinical work.
R2C2 was originally developed for feedback conversations grounded in data, but it’s equally useful for guiding a reflective discussion after a direct observation.
Ask–Tell–Ask: The Foundational Feedback Loop
Framework Outline:
-
Ask the learner for their self-assessment.
-
Tell your observations of specific, modifiable behaviors and their potential impact (positive or negative).
-
Ask again for interpretation, ideas, and/or next steps.
→ Repeat the loop as needed for different aspects of performance.
This framework keeps the learner thinking, not just listening.
It starts with curiosity, adds observation, then circles back to reflection and next steps.
Example – Procedural Skill (Elliptical Incision)
ASK: “How do you think that went?”
Learner: “Pretty good. I was paying attention to my 3:1 incision ratio.”
TELL: “You did a near-perfect job with the ratio; your hand was steadier than last time.”
ASK: “What do you attribute that success to?”
Learner: “I measured, marked, and focused on precision.”
ASK: “What else went well or what would you do differently next time?”
Learner: “I can’t think of anything.”
TELL: “One thing I noticed? You didn’t check in with the patient until it was over. They might feel more supported if you do that earlier.”
ASK: “How could you do that and still keep your focus next time?”
The learner might suggest involving the MA or offering a quick check-in mid-procedure or come up with something you’ve never considered.
That’s the gold of this approach: it keeps the feedback practical and learner-driven while reinforcing that this isn’t about judgment, it’s about growth. Focusing that last question on the next time can help them not ruminate and see it’s all about mastery and growth.
R2C2: Building Relationship and Shared Meaning
While R2C2 was originally designed for making meaning from compiled feedback data, it also works beautifully in direct observation when the goal is to deepen reflection or connect observed performance to broader reasoning patterns.
Example – Direct Observation (Neurologic Exam)
-
Relationship: “I’m glad you invited me to observe your neuro exam. I’ve noticed you’re being intentional about sharpening that skill, and I appreciate your openness to feedback.”
-
Reaction: “How did that feel to you?”
Resident: “Honestly, clunky. I think I covered most of it, but I lost my flow midway.” -
Content: “You’re right. You did cover most of it. Your cranial nerve testing was smooth and systematic. During the senory portion, I noticed you switched tools twice and you said ‘tell me if this feels different’ before explaining different from what.” It wasn’t clear to me if the patient understood “different from what.”
-
Coaching: “What might help you keep your flow and clarity there?”
Resident: “Probably thinking out loud for a moment before starting and orienting the patient first.”
Faculty: “That’s a great idea. That sounds like a tool often used called a quick ‘verbal roadmap’, telling the patient and yourself what’s next. It keeps you organized and the patient engaged. How could you test it out?Resident: Well, my next patient is an annual wellness visit, I could just practice it then.
Faculty: Great plan! And how will you know if it’s useful?
Resident: Well, if I’m a bit smoother and the patient seems clear, it’s a step in the right direction.
Faculty: What else might you want to do between now and then?”
Resident: I’m going to briefly think through the flow of the exam and tools before going in.
Used this way, R2C2 turns feedback on a physical exam from a list of corrections into a shared sense-making process that builds confidence, precision, and adaptive expertise.
Prepare to ADAPT: Coaching in Real Time
This one shines in real-time observation and feedback.
Example – Direct Observation (Patient Communication)
Learner (Prepare):
“I’d like feedback on how I explain the treatment plan when the patient has a lot of questions, which this patient always does.”
Coach (Prepare):
“Great, so I’ll observe with that in mind, jot a few notes, and we’ll debrief right after. Does that sound good?”
(During the visit, the resident performs while the coach observes neutrally.)
Ask → Discuss
Coach: “How did that feel from your perspective?”
Learner: “I think I was clear, but I could tell she was starting to tune out.”
Coach: “That awareness is key, I noticed you were very thorough, clear, and accurate, but she did seem to look away after about a minute. One small shift that can help is to pause after your first explanation and ask, ‘What questions do you have so far?’ It signals partnership and lets you recalibrate in real time.”
Learner: “That was my plan, but maybe I need to do it earlier. What other things could help?”Coach: “Another trick I use is to summarize in one sentence first, then ask for how much detail they’d like. For example, ‘We’ll start a new medication to control your blood pressure; would you like to hear how it works or just what to expect?’ That keeps the conversation efficient and patient-centered.”
Plan Together
Coach: “Of the ideas we discussed, which one feels like the best fit to try next, or did something else come to mind while we were talking?”
Learner: “I think I’ll try starting with a one-sentence summary and then check for understanding.”
Coach: “Great. How will you know it’s working?”
Learner: “I’ll pay attention to whether patients can restate the plan accurately and seem more engaged during the explanation.”
Coach: “Excellent, let’s follow up in a week or two and see how that goes.
This short interaction shows the Co-Creation Zone in action — a blend of curiosity, reflection, and faculty guidance.
A Note on Frameworks
Each of these frameworks, Ask–Tell–Ask, R2C2, and Prepare to ADAPT, offers a different rhythm for the same goal: turning feedback into insight, learning, and growth.
They’re not mutually exclusive or ranked by importance. Some faculty prefer to pick one and practice it until it feels natural; others flex among them based on context.
Think of them like instruments in the same orchestra: the more fluent you become, the easier it is to improvise.
-
Ask–Tell–Ask may feel easiest for short feedback moments.
-
R2C2 deepens the conversation when you have more data or want to explore reasoning.
-
Prepare to ADAPT works beautifully for real-time observation and feedback.
The “best” framework is the one you’ll actually use, consistently, thoughtfully, and with curiosity. Once the rhythm feels natural, you’ll find yourself blending them without even thinking about it. That’s when coaching becomes a habit, not a skill you have to remember.
Everyday Coaching in the Real World
And remember, coaching doesn’t always need a full framework.
Sometimes, in a busy clinic, coaching is as simple as asking something you likely already use:
“What’s your clinical question?”
That one line turns on the learner’s self-reflection muscle, it forces synthesis and helps them articulate what they’re noticing or uncertain about. They’re tuning into Schon’s surprise. Then you can answer or look it up together if it’s needed in the moment.
Lately, I’ve also taken the time to model it back, both as a model of self-reflection and to normalize we often have questions no matter how much experience we may have. My most recent:
“My clinical question is what’s the data on repeat injections for carpal tunnel syndrome? Does the effectiveness rate change, and how do repeat injections affect avoiding or delaying surgery, if at all?”
When learners hear that kind of transparent thinking, they start forming their own internal script for curiosity and growth.
Why It Matters
Performance coaching sits at the heart of faculty practice. You are guiding learners toward better performance and stronger self-direction.
When done well, it builds more than competence: it develops reflective, adaptive physicians who can learn from every patient encounter, feedback moment, and surprise. That will keep them adaptive in the coming years! And, the bonus is it helps them see you as a partner in their learning, not a judge passing harsh judgment that send them in a spiral - which is good for everyone's wellbeing.
That’s the real power of coaching, not always the content of what we teach, but how they learn to identify gaps, and teach themselves.
Next week: Putting it all together. The Adaptive Coaching Spectrum: Becoming a Master Adaptive Faculty
How to recognize where you are on the coaching continuum and when to flex left or right based on the learner, relationship, and context.
Join Weekend Reads
Weekly insights, tips, and tools for physicians who want to thrive—plus a dash of fun.
We hate SPAM. We will never sell your information, for any reason.

