
Physician Coaching and Mentoring as a Core Faculty Member
We are in a series of blogs looking further into coaching and mentoring and how they differ. This week is intended for core faculty bringing a more intentional coaching approach to your trainees (and colleagues) - Thank You!
If we knew nothing more than that leading companies in the corporate world have invested heavily in coaching for their C-suite over decades, we would know enough to realize the importance of bringing it into the medical field, another high-stakes profession. (Large successful corporations rarely waste money for decades on unsuccessful investments). We might also rightly suspect that incorporating coaching early in the process is crucial. We actually do know the impact coaching affords medicine. The studies on physician coaching and coaching in academics are small but growing. There are larger randomized multi-center trials currently taking place.
And that's not all. In addition to extrapolating from corporate America and an increasing number of studies, national leaders use and promote coaching in medical education.
NAM's National Plan for Health Workforce Well-Being provided an expert panel. (You can watch the proceedings where Dr. Vivek Murthy, Dr. Victor Dzau, Dr. Chris Sinsky, Dr. Chris Cassell, and several other leaders discuss the actionable plan and its importance). When asked how we set the medical culture to be self-forgiving, not foster impostor phenomenon and make it okay to say," for these job demands, I need these resources," Dr. Christine Cassel, UCSF Professor of Medicine, gave two key actions. The first dealt with the educational process, with mindful attention being given to the impressions conveyed to trainees, including the 'hidden curriculum.' The second was "to create a universal availability of coaching for every student once a month, more than that if they want. We learn that from the business community, where high-power executives under a lot of pressure are expected to seek coaching, expected to ask for help and feedback about how to deal with difficult situations. That is an important step for medical schools to normalize and have it be available for the faculty as well. So, it becomes part of the culture of medical education."
So, thank you, core faculty, for 1. Showing up. 2. Growing in your coaching skills and integration, and 3. Meeting trainees where they are. You are tuning into your intuition about when to direct, when to coach, when to suggest, when to advocate, and when to just listen. And you're doing it all during some of the most challenging times for medical professors. I'm hoping the ACGME, NBME, and Academic and Community sponsoring training institutions will awaken to the support you need to usher in the next generation of phenomenal and flourishing physicians.
Last week, I highlighted the 5 main hats you wear as you relate to your trainees - 1. Cinical Educator 2. Sponsor 3. Mentor 4. Advisor 5. Coach. There are situations that call for one approach above another. For instance, we know from UW's Prepare to ADAPT model, that coaching is incredibly effective for feedback. I capture the concept of the various roles in the model below. As I see it, you already bounce in and out of one method of relating to any given resident at any given time, and at other times, you blend approaches.
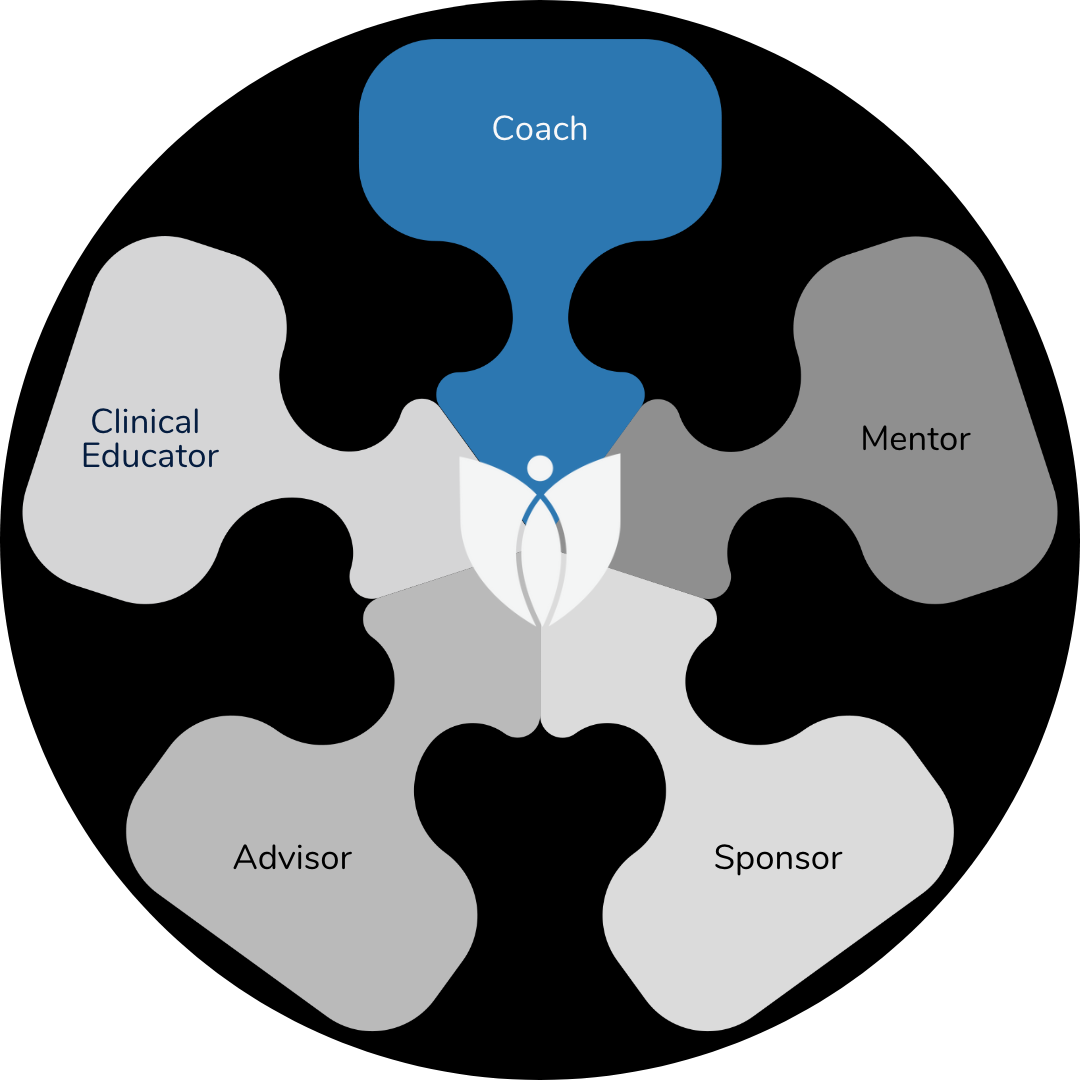
I often reflect on two other interesting phenomena in how it relates to the minimum of five various trainee relationship roles that you play. One is the concept of how you really bring your whole self. Yes, you may mentor in one setting by guiding and directing based on your experience; in another, you may hold space, listen and ask probing questions for residents to access their best answer. But you can't unknow what you know from your various hats. I suspect that a functional MRI scan may show five distinct areas lighting up as you meet with a resident, with one focus shining more brightly as you lean into a specific way of relating that seems best. You will become more skilled at what approach or blend to take with any given trainee at any given time. It'll become fluid.
In a similar vein, I was coaching a dear friend in a tough spot because she asked me to assume that role. I wanted to assist in that manner. I'm pretty good at a rigid boundary and setting aside things that would sidetrack my coach brain. At the end of the last session, she asked me what I thought. I told her that it is so much more important what she thinks. She asked me again. I asked if she was asking me as a coach, a friend, or a doctor. She said, "I need the whole you please." It's true; we aren't really fragmented into various roles. And that is one exceptional thing about being core faculty interacting with trainees. You bring ALL of you.
The second is the evolving nature of your roles. They're dynamic over time. I have former residents that are my friends. I have former mentors that are friends. I have many former residents that are colleagues – and two have become my bosses! Those of you in this role for any length of time have likely become graceful as your interrelatedness unfolds. You allow yourself to ebb and flow into the natural progression of the connection. That's one more awesome thing about your role!
Next week, I will examine what coaching and mentoring look like for external physician coaches and trainees and the approaches to making the most of your sessions.
Until then, have a joy-filled day! Tonya
Learn how I partner with family medicine residencies as a coach.
Join Weekend Reads
Weekly insights, tips, and tools for physicians who want to thrive—plus a dash of fun.
We hate SPAM. We will never sell your information, for any reason.

